Teilnahmebedingungen für das Gewinnspiel “Brain Boost Event 2025 – Gewinne 2x Teilnahmeplätze für dich und deinen Lieblingskollegen in Seefeld”
Teilnahmebedingungen:


Zirconia may be part of your everyday vocabulary, but how much do you know about this ceramic material? Learn more about the “why’s” of 3Y, 4Y and 5Y zirconia, which to use, and when – and how you can take advantage of its benefits for chairside dentistry.
Alumina oxide, synthetic glass-ceramics, feldspathic-based ceramics, zirconia – when it comes to ceramic and ceramic-like restorative materials, dentists have a lot of options. And while each material has its own set of advantages and drawbacks, zirconia-based materials have been a popular choice for years due to their high strength, wear resistance, availability, and moderate cost.
However, despite the category’s popularity, there’s still some confusion about what makes zirconia unique – including the different forms it takes, its bonding procedures, and what it brings to the table esthetically.
Much of the confusion surrounding this material has to do with its name. The word “zirconia” has many associations, including a mineral (zircon, or zirconium silicate, ZrSiO4), an atomic element (the metal zirconium, Zr), and even a synthetic gemstone (cubic zirconia) – making it very easy to misunderstand what makes dental zirconia dental zirconia. To make matters more confusing, dental zirconia itself is known as “zirconium dioxide,” “zirconium oxide,” as well as simply “zirconia.” And while dentists may also affectionately refer to it as “white metal” or “ceramic steel” due to its strength, it’s not a metal. In fact, it’s actually a good alternative to metals.
Let’s start with the element Zirconium, a very strong but malleable silvery-white metal that resists chemical corrosion (making it bio-inert), with chemical and physical properties similar to titanium.1,2 However, Zirconium isn’t found in nature in its pure form, and instead is found and mined as multi-element minerals like Zircon.3 These minerals are then refined and purified to produce zirconium intermediates, e.g. zirconium oxide powder. From there, different oxides are added to the powder to stabilize the result (which will be discussed more later), ultimately producing the biocompatible and adaptable dental material, zirconia. The powder is then pressed and shaped into porous pucks or blocks with about 50% of the full density of zirconia. Thermal treatment is required to get the right material hardness, so these pucks or blocks are milled to create restorations. However, these milled restorations still have some porosity. Only the final sintering step can transform the material into fully dense, strong, and biocompatible dental zirconia.
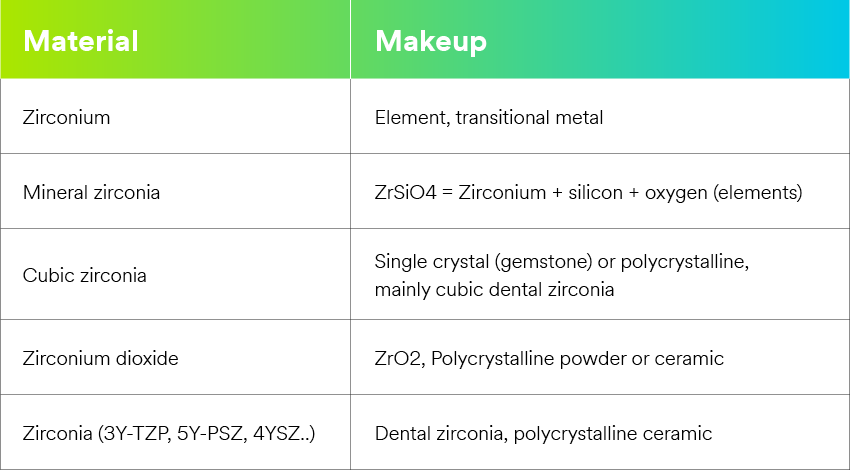
Today, many types of dental zirconia are available from a number of manufacturers, each with their own unique brands and product names – making it that much more difficult to choose among them. The fact is that all dental zirconias have fairly similar compositions. The differences lie in how they are made: differences in heat, pressure, and added metal oxides. To understand which zirconia is best for your procedure, it’s important to know what goes into the material.
Phases
Pure zirconia is a polymorphic ceramic, meaning that depending on temperature and pressure, it can exist in three different crystallographic structures – monoclinic, tetragonal, and cubic.
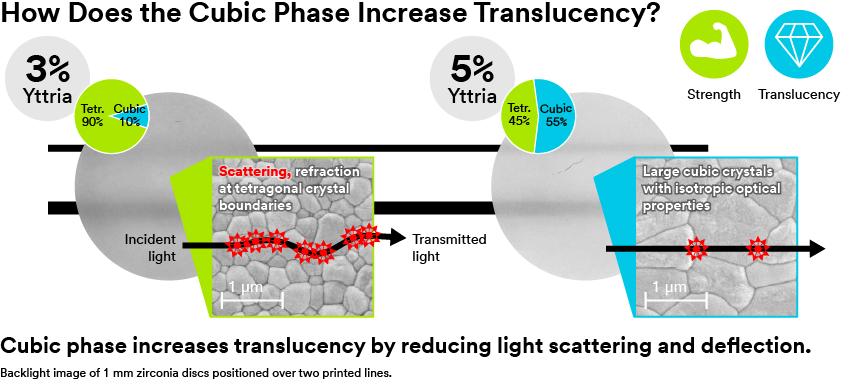
At room temperature, pure zirconia is in the weaker monoclinic phase. As the material is heated, it transforms into the tetragonal phase. With even more heat, it reaches the cubic phase. However, as the material cools, it will return to earlier phases – unless stabilizers are added. Depending on type and amount, these stabilizers can keep the tetragonal or cubic phase stable at room temperature. These stabilized phases are more mechanically sound and result in different optical properties. Stabilized tetragonal zirconia is tough but has lower translucency. This is because its structure is birefringent, meaning it has multiple refractive indices, which scatter and deflect light – reducing translucency. Stabilized cubic zirconia, on the other hand, has a symmetric structure, allowing light to pass through more easily, improving translucency. Unfortunately, this optical improvement comes at the cost of mechanical properties, which begin to decrease.
Metal oxide stabilizers
Despite how tough zirconia is, if you were to make a ceramic from its pure form, it would result in a weak restoration. Much like iron, zirconia requires certain additives to stabilize and strengthen the material and improve its mechanical, esthetic, and optical properties.
The most common dental zirconia formulations include yttria, a metal oxide, to stabilize the tetragonal and cubic phases of zirconium. Yttria, when built into the lattice, transforms the crystal structure of zirconia to provide strength and optical properties. However, the amount of yttria added makes a difference.
Yttria is added to zirconia in small amounts (mol.% yttria), indicated by a number and the letter ‘Y.’ When it was first introduced, almost all zirconia was 3Y, tetragonal, and fairly strong (<1000 MPa) but with low translucency. (Alumina was included in some formulations to help sintering and stability but was subsequently reduced in future generations. In succeeding material generations, yttria content increased to 5Y (5 mol.% yttria), providing higher translucency but lower strength due to more cubic phase polycrystals. More recently, 4Y (4 mol.% yttria) formulations have been developed, providing a good balance of high strength and translucency – so much so that 4Y could be called a “universal” or “high translucent” zirconia.
Based on what yttria can do to zirconia in various concentrations, dental manufacturers are modifying the chemistry involved to find the optimal balance of final properties. As such, many different types of zirconia are available. Knowing what each brings to the table can help you make the best decision for each case.
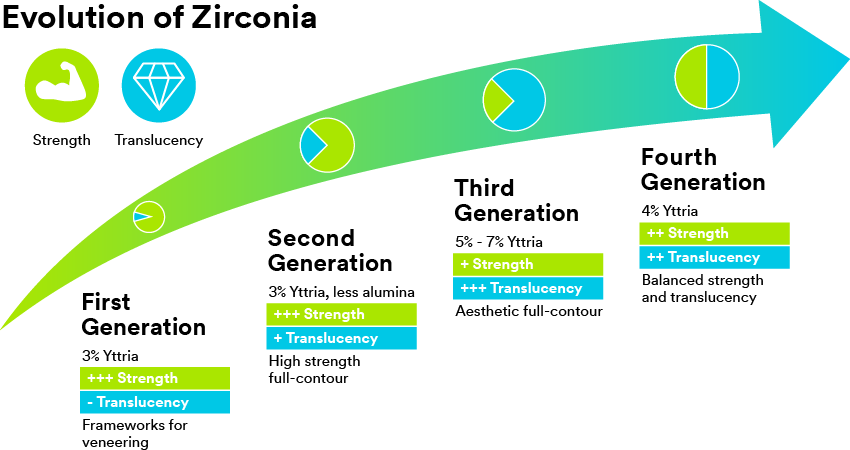
Zirconia is not a “one-size-fits-all” solution; rather, different materials offer different levels of strength and translucency. Which zirconia is best for you ultimately comes down to your treatment’s esthetic and mechanical needs.
In the past, dental zirconia simply wasn’t very esthetic and required additional steps to achieve a natural-looking result. As the material has advanced, however, so has its esthetic potential. With this in mind, it’s still important to select the right formulation for each case. If esthetics are most important and strength isn’t an issue – such as an esthetic anterior restoration or pre-molar with room for thicker walls – a higher translucency zirconia, such as 5Y zirconia, would be best. Alternatively, when strength is vital – such as posterior restorations or multi-unit bridges – a second-generation, 3Y zirconia would be more appropriate. And while there is no true “universal” zirconia, fourth generation, 4Y zirconia provides a versatile balance of properties for a variety of procedures. Beyond yttria, esthetics can be further enhanced with color shading, either by using pre-shaded zirconia or staining the restoration after placement. The highest esthetics can be achieved by using veneer ceramic over the zirconia coping.
Minimally Invasive Versatility
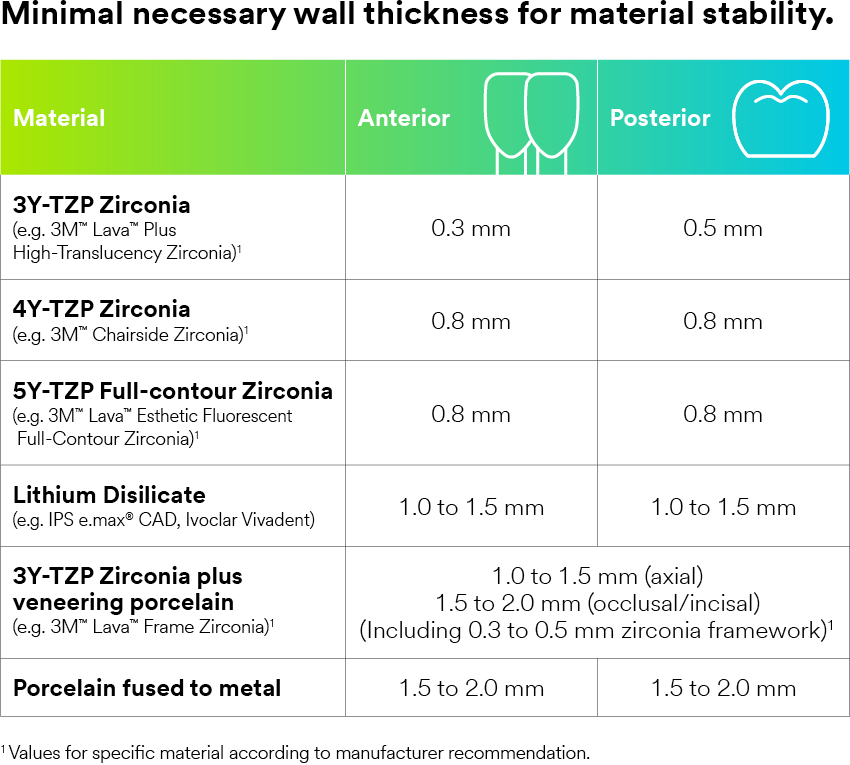
In addition to these esthetic advancements, modern zirconias complement a more conservative dental philosophy. Lower strength restorative materials require more bulk, or a wall thickness of 1mm or more*, to support the restoration. As a result, more sound tooth structure needs to be removed to create space. However, because zirconia provides more strength, restorative integrity can be achieved with thinner walls – enabling less invasive preparations.
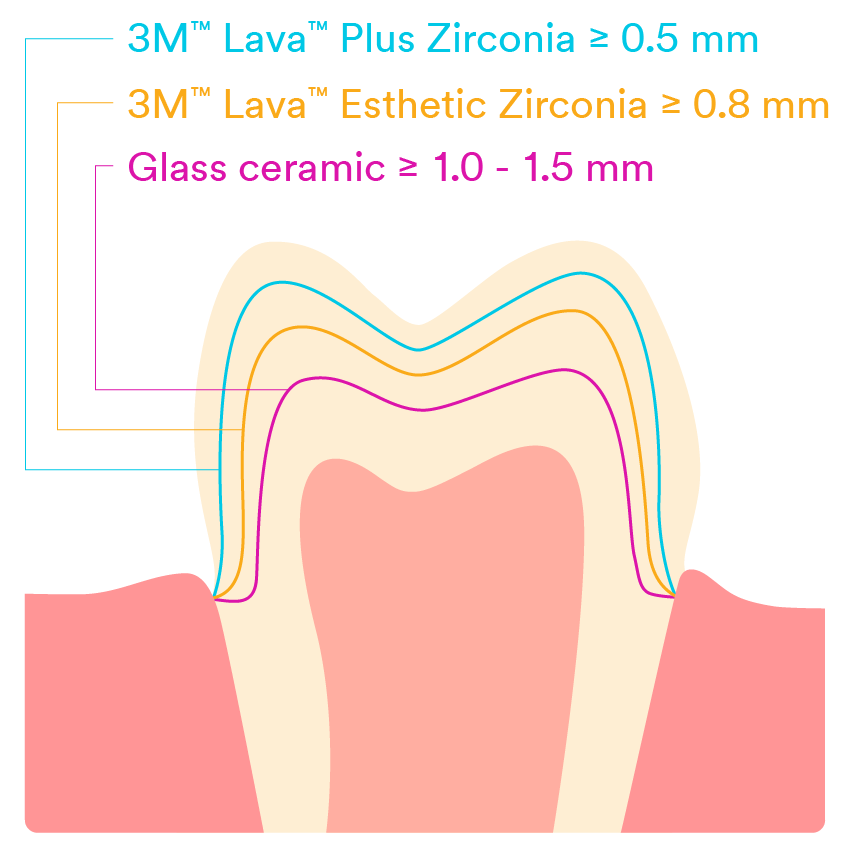
Minimal wall thickness for crowns for different material options.
With all of this in mind, zirconia is still evolving as manufacturers continue to pursue even better esthetics, thinner walls, and shorter sintering times. Zirconia is already biocompatible, and modern formulations offer such a favorable balance of esthetics and strength that material advancements have only made it that much more advantageous. For example, some materials, like 3M™ Lava Esthetic Fluorescent FullContour Zirconia, feature pre-shaded, built-in fluorescence for a more natural result – instead of an added fluorescent glaze that can wear off over time.
Chairside Zirconia
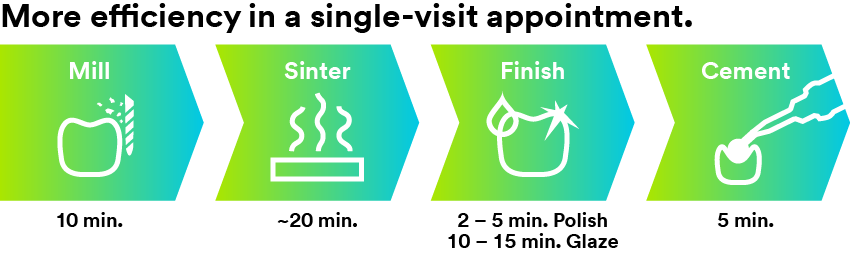
Temporary restorations, working with a lab, return visits for fitting and proper seating… traditional zirconia restorations can be time-consuming procedures. Plus, patients have to endure long wait times and the potential for more pain. Thankfully, in addition to more esthetic, minimally invasive formulations, zirconia has also entered the chairside landscape.
The advent of chairside zirconia has created an opportunity to produce high-strength, esthetic restorations on the same day – no temporaries, multiple visits, or lab needed. A full-digital workflow gives the ability to visualize, analyze and track treatments. It also offers fine control over design and close collaboration between patient and dentist. And because the restoration is produced in-house, without outsourcing to a lab, there’s less risk of miscommunication – and revenue stays in the dental office.
Cementation of Zirconia
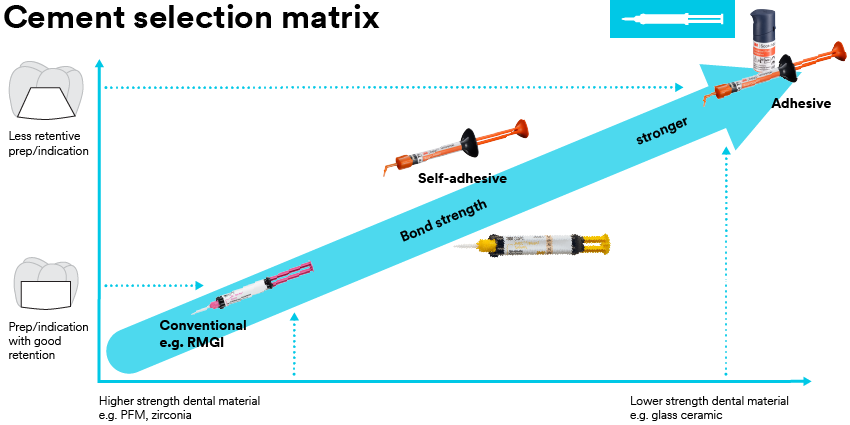
A high-strength ceramic material like zirconia is only as good as its bond, and that means paying careful attention to cementation protocols. It’s important to note that the bonding protocol of zirconia is different than other ceramics – in fact, it may actually be easier.
Unlike other ceramics that require many preparation steps to ensure a strong bond, zirconia restorations with adequate retention and ceramic material thickness can be cemented conventionally without many technique-sensitive bonding steps. Adhesive bonding is only required in situations with limited mechanical retention. This applies regardless of zirconia generation. When bonding, it’s critical to remember that zirconia should not be etched, even to remove saliva after try-in. This is because phosphoric acid – and the phosphate in saliva – can block the oxide groups necessary for bonding.4,5 In terms of pre-treatment, zirconia restorations should always be sandblasted prior to final placement. Once clean, the cement can directly be applied, and the restoration can be seated.
With all of the above in mind, the best cementation technique for your zirconia restoration is dependent on the preparation, and its retention. For example, if you’re using zirconia for a veneer (where esthetics are key and a weaker, more translucent zirconia is best), or in situations with limited mechanical retention, adhesive cementation may be more appropriate. It’s a matter of balancing qualities to achieve the best results possible.
While there are many materials for dental professionals to choose from, zirconia continues to grow as a category. It’s evolved from simply a strong restorative option to a material with newfound esthetics and minimally invasive potential -– a material worth exploring. However, these advantages can only be accessed when one has a thorough understanding of zirconia’s unique chemistry, what each generation brings to the table, and how their strengths can complement your procedure.
SOURCES:
1. “Zirconium Dioxide (Zirconia): Properties, Production and Applications.” Matmatch, https://matmatch.com/learn/material/zirconium-dioxide-zirconia.
2. Alex, Gary. “Zirconia – Separating Fact from Fiction.” Oral Health Group, 2 July 2019, https://www.oralhealthgroup.com/features/zirconia-separating-fact-from-fiction/.
3. Saridag, Serkan, et al. “Basic Properties and Types of Zirconia: An Overview.” World Journal of Stomatology, Baishideng Publishing Group Inc., 20 Aug. 2013, https://www.wjgnet.com/2218-6263/full/v2/i3/40.htm.
4. Götzinger, Martin. “Exposing 3 Myths about Zirconia.” 3M Dental Blog, 25 Aug. 2020, https://dentalblog.3m.com/dental/exposing-3-myths-about-zirconia/
5. Blatz, Markus B, and Julian Conejo. “Cementation and Bonding of Zirconia Restorations.” Aegis Dental Network, 1 Oct. 2019, https://www.aegisdentalnetwork.com/cced/specialissues/2018/10/cementation-and-bonding-of-zirconia-restorations.

How do you motivate your patients? Discover how caries risk assessments and motivational interviewing tactics can help you connect with…
Caries is a complicated multifactorial disease. In this two-part series, explore how caries risk assessments can help improve evaluation and…