Teilnahmebedingungen für das Gewinnspiel “Brain Boost Event 2025 – Gewinne 2x Teilnahmeplätze für dich und deinen Lieblingskollegen in Seefeld”
Teilnahmebedingungen:

Now more than ever, dental professionals want ways to work more efficiently and conservatively. Learn how innovative techniques and materials work together to promote minimally invasive restorative procedures.
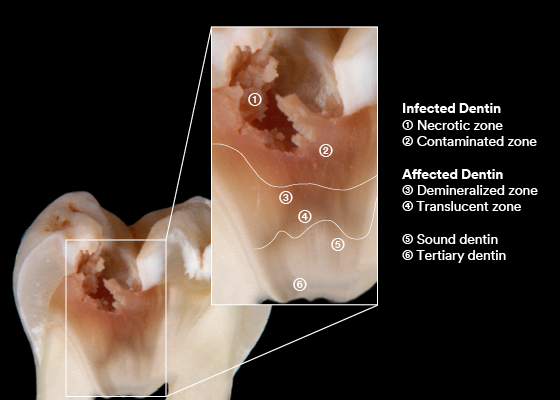
Caries zones – Image courtesy of Prof. Leandro Hilgert and Prof. Soraya Leal, University of Brasilia (UnB), Brazil.
Not all carious lesions are alike: they differ in size and location, caries activity, cavitation and cleanability. The latter three factors determine whether a lesion is likely to progress quickly, which may lead to further damage of tooth structure and future loss of function. In order to act as conservatively as possible, it’s important to respect these factors when determining whether any form of invasive restorative treatment is necessary.
In a recently published expert consensus statement on minimally invasive dentistry (MID), it’s recommended to only resort to invasive treatment strategies in two scenarios:
In the proximal area, which is not easily visible and accessible with instruments, the extension of the lesion should be assessed with the aid of a radiograph. Whenever the core or inner third of the dentin is affected, it’s likely the lesion is cavitated, and an invasive treatment is necessary. In other cases, it’s usually possible to adopt micro-invasive treatments – such as sealing or caries infiltration – or even non-invasive strategies. Recommended non-invasive measures include professional biofilm management, topical fluoride therapy and calcium and phosphate application to aid remineralization.
If treatment is required due to a defective restoration, the dental practitioner should opt for repair rather than replacement whenever possible.2,3 When the clinical condition of the tooth is in question, or a particularly high caries risk or other factors make it necessary to replace the restoration, additional removal of tooth structure should be minimized as much as clinically possible.
If a lesion requires invasive restorative treatment or an existing restoration needs to be replaced, selective caries removal is the technique of choice.4 In most cases with lesions of low to moderate depth, the soft carious dentin (also referred to as caries-infected dentin) is removed completely, while the firm (caries-affected) tissue is left untouched – except in marginal areas. Excavation up to hard dentin in these areas ensures a tight seal of the restorations. Whenever soft dentin is found close to the pulp, infected tissue should be left untouched to avoid pulpal damage. Discolored dentin below amalgam restorations may also be maintained. In fact, research has revealed that this dentin contains corrosion products and is demineralized, however it has been shown that it does not need to be removed.5 The staining is mainly due to the presence of tin and zinc, which may actually have a positive effect on the substrate.6
The success of minimally invasive restoration techniques is highly dependent on the use of high-performance dental materials, which give dental practitioners more control over the process. Adhesives and filling materials need to form a tight seal and should be biocompatible and easy to use for high procedural safety. For minimally invasive restorative and repair procedures, universal adhesives are a great choice.
3M™ Scotchbond™ Universal Adhesive with MDP (10-Methacryloyloxydecyl dihydrogen phosphate) allows for better performance on dentin, improves product stability, and offers adhesion to metal and non-glass ceramic substrates.
Now the manufacturer has released a new version with some added features. 3M™ Scotchbond™ Universal Plus Adhesive has a BPA-derivative free formulation and is radiopaque. It features dentin-like radiopacity to help reduce the risk of misdiagnosis in case of adhesive pooling. It also bonds and seals affected dentine, supporting minimal invasive dentistry.
The following case example illustrates a minimally invasive restoration replacement procedure using 3M™ Scotchbond™ Universal Plus Adhesive.
In 2010, an insufficient amalgam restoration in this first molar was replaced with condensable composite. Ten years later, it was again necessary to take action. Wear of the disto-occlusal surface resulted in dentin exposure in the composite restoration. The remaining enamel on the occlusal surface is visible. Due to sensitivity issues, the restoration was required. In addition, recurrent caries could be observed. Another contributing factor was the loss of occlusal contact caused by previous orthodontic treatment. The decision was made to reconstruct the tooth with a minimally invasive direct composite restoration.

Occlusal view of the initial situation on lower first molar.

Bitewing radiograph of the initial situation.
In the present case, the carious-affected dentin was left at the center of the cavity according to minimally invasive preparation guidelines.
Intact occlusal enamel was left untouched. To protect the adjacent tooth, a matrix band was placed and secured with a ring. Subsequently, the enamel was etched with a phosphoric acid gel for 15 seconds, and rinsed with water. For bonding, the new 3M™ Scotchbond™ Universal Plus Adhesive were actively applied to the moist tooth structure before being dried with a gentle stream of air to ensure solvent evaporation. Active application, i.e. massaging of the material into the tooth structure, improves the material’s performance.7,8 Adhesive was then light cured for 10 seconds.
The tooth structure was restored using a BPA-free composite resin (3M™ Filtek™ Universal Restorative). Finishing and polishing was accomplished with the aid of the 3M™ Sof-Lex™ Diamond Polishing System.

Active application of 3M™ Scotchbond™ Universal Plus Adhesive.

Light curing of the universal adhesive.

Build-up of the proximal wall with the aid of a sectional matrix system.

Occlusal view of the restored tooth prior to polishing.

At the one-month recall, the restoration was examined clinically and tested for sensitivity. The patient turned out to be free of symptoms.
It is well accepted nowadays that bacteria cannot be completely removed by preparation. Therefore, “The seal is the deal”: A successful restoration will cut off any remaining bacteria from nutrients and stop caries from progressing.9
The above case not only demonstrates a minimally invasive restorative approach, but also highlights the benefits of innovative dental materials in this context. 3M™ Scotchbond™ Universal Plus Adhesive contains MDP and is able to bond and seals caries affected dentin. Hence, this new universal adhesive helps us to support reliable outcomes of less invasive treatments.
Sources

How do you motivate your patients? Discover how caries risk assessments and motivational interviewing tactics can help you connect with…
Caries is a complicated multifactorial disease. In this two-part series, explore how caries risk assessments can help improve evaluation and…