Managing caries and motivating change, part 2: Motivational interviewing
How do you motivate your patients? Discover how caries risk assessments and motivational interviewing tactics can help you connect with…

Whether taken digitally or physically, a good dental impression is key to restorative success. But how do you decide which method or material is best for each case? Discover what to take into account to achieve clinical success.
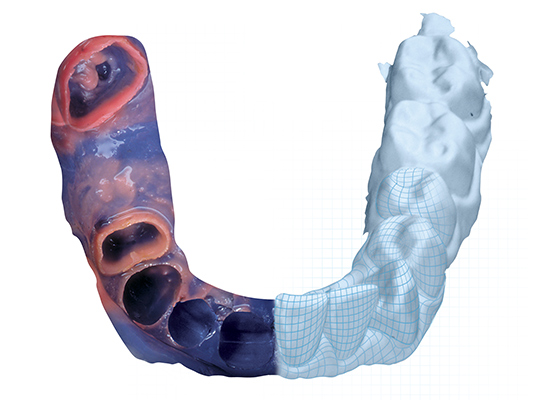
Impressions, whether digital or physical, will make or break a restorative case. I started 25 years ago with digital restorative dentistry and today utilize digital means for most of my restorative and appliance dependent cases. Does that mean that physical (analog) impression materials have diminished in relevance or are on their way to becoming obsolete? Are intraoral scanners superior to analog materials? Does economics favor one over the other? Is the hype greater than the reward? What are the preferences of dentists, laboratories, and patients? Can you be 100 percent digital, and will it make you a better clinician?
Dental marketplace statistics indicate interest and adoption for intraoral scanners (IOS) accelerating when used for the sole intent of digital impression transmission to laboratories. Intraoral scanners are seeing more interest and rapid adoption than their progenitor, chairside CAD/CAM systems, because most dentists still prefer laboratory support despite the known advantages of the chairside CAD/CAM fabrication.
Whether analog or digital, clinical success is primarily dependent on the quality of the data (physical or analog impression).
I utilize two intraoral scanners, have and continue to perform chairside CAD/CAM (since 1995), and I have also had experience with most major IOS devices. Despite my digital legacy, I still use physical materials because they can pick up the slack when digital materials fall short. These materials have a long history of clinical success and can also be more efficient in certain cases. Rather than tell you to use one or another, I encourage you to focus on evidence and performance, whether it is with a device, material, or your own hands. The real question is: How do we optimize each material and where are they best applied?
Beginning with physical materials, let’s identify the properties needed for a “universal” or ideal impression material. Typically, we need:
While not totally inclusive, no one such perfect material exists creating the need for multiple materials.
With IOS the ideal equipment would command:
In this piece I will represent both digital and physical materials along with the comparative skillsets required by each.
Current evidence in the literature cautions or contraindicates the following for IOS:
I also prefer physical materials for the following:
When it comes to edentulous and partially edentulous patients, I would think most US dentists would use a VPS or polyether material, with VPS in the clear majority. I won’t argue that excellent results cannot be achieved using both, but I will state that polyether (PE) has distinct advantages, and, in my experience, VPS falls a bit short. This is why PE has been my go-to material for over 25 years where IOS is not indicated (edentulous and partially edentulous).
PE is inherently hydrophilic and exhibits the lowest water contact angles of all elastomeric materials. VPS materials, by comparison, have surfactants added to them to lower the contact angles, but they are not equivalent to PE. I’ve tried many VPS materials over the years and always go back to PE, especially with today’s formulations which have by and large addressed tastes, odors, difficult removal, and long set times. As an inherently hydrophilic material, PE excels in terms of flow. It has the inherent wettability necessary for the reproduction of the finest details where success is measured in microns. And let’s be real, moisture forgiveness is a big deal!
For these reasons, when physical materials are needed, PE satisfies all my needs for fixed and removable prosthetics. Laboratories that I have worked with over the years also generally report fewer remakes with PE as compared to VPS. Full arch cases and frameworks for fixed or removable prosthetics demonstrate precision fits. PE is available in varying viscosities and I prefer “soft” quick polyether materials with a syringeable light body, which is much easier to remove from undercuts. My ideal set time is 3:00 minutes (a regular set of 4:15 is also available). Soft, quick polyether materials are applicable for the largest and most routine of cases. In terms of delivery, I prefer the centralized, automated mixing system as opposed to the gun-cartridge system.
I do use VPS in one situation – for gaggers and behavioral patients, where speed is paramount and clinically sufficient detail can be realized. Imprint 4 Super Quick (set time 1:30) is great for single units and a lifesaver for problematic patients needing partials and dentures (custom tray recommended).
The literature supports the premise that dental appliances and fixed prosthetics can be successfully accomplished using digital or physical material techniques with no clinically significant differences in outcomes, though physical material has the highest degree of capability. Technique and application can be the doctor’s Achilles heel, as such, I offer these points for consideration:
The literature, along with my own experience, does support the following claims for IOS:
If you operate with physical materials only, you are already 100 percent capable, and your results can mirror that of any IOS device if you achieve retraction, can account for oral fluids, and address the challenges associated with physical materials vs. the challenges for a camera. If you already use or are contemplating using an IOS device, physical materials are also needed because digital impressions lack 100 percent capability.
What does separate IOS devices is their overall functionality in today’s rapidly growing dental and digital workspace. Where a practice fits into this equation today or in the future is unique to each organization. When considering comparative costs, future enhancements, patient acceptance, overall efficiency, ease of use, and intangible benefits, these systems are getting more comparable; especially as capabilities expand.

How do you motivate your patients? Discover how caries risk assessments and motivational interviewing tactics can help you connect with…
Caries is a complicated multifactorial disease. In this two-part series, explore how caries risk assessments can help improve evaluation and…

Zirconia may be part of your everyday vocabulary, but how much do you know about this ceramic material? Learn more…