Teilnahmebedingungen für das Gewinnspiel “Brain Boost Event 2025 – Gewinne 2x Teilnahmeplätze für dich und deinen Lieblingskollegen in Seefeld”
Teilnahmebedingungen:


How do you motivate your patients? Discover how caries risk assessments and motivational interviewing tactics can help you connect with and inspire your patients to make real change.
As discussed in part one, caries risk assessments are a valuable tool for modern dental practices with a variety of benefits for you, your team, and your patients. However, these assessments can only do their best work if patients understand, accept, and follow through with your recommendations – which is easier said than done.
Thankfully, there are counseling methods designed to help you get to know your patients at a deeper, more empathetic level and educate and motivate them to make real changes. In this article, we’ll explore motivational interviewing techniques to help make the most of your caries risk assessment and improve patient relationships, acceptance, and compliance.
While caries risk assessments identify and track patient risk factors and help personalize treatment, several patient factors can still prevent the assessment from reaching its full potential. Each patient’s oral health literacy, circumstances, and motivation can impact their openness to change.
When using an assessment tool, it’s important to explain not only what the assessment is but also why you’ve decided to use it. Every patient has a unique level of oral health understanding and it’s critical to determine what your patient already knows and fill the gaps thoughtfully and individually. Acceptance is the next hurdle. Patients may not accept preventive treatment for many reasons, but individualizing their care can help you discover and overcome their barriers to treatment. Show them their unique risk assessment and take time to explain and answer their questions. Patients are more likely to accept treatment if they feel seen and involved.
However, even if patients accept treatment, they can only make progress if they follow through at home. Beyond tracking risk factors, taking the time to learn your patients’ motivators, circumstances, and barriers can help you present the most appropriate recommendations– after all, there is no one-size-fits-all approach. Acceptance and compliance take time, but by finding what motivations patients and encouraging them consistently, you can help inspire change.

Caries assessments work best when patients are honest – but getting them to open up isn’t always simple or easy. Fear and shame are common for dental patients, and it’s not unusual for them to lie about their habits or health history. In fact, according to a DentaVox survey, 73% of patients have lied to their dentist.1 How do you encourage patients to be honest so that you can use your caries risk assessment to the fullest and provide the best care possible? By building a relationship of trust. However, building trust can be tough. As dental professionals, we often must be the bearers of bad news. Of course, none of us want to hurt patients’ feelings, but we also can’t do them the disservice of sugarcoating the facts. We must strike a balance between ensuring patients understand the diagnoses and its importance – without adding barriers of shame. It’s also important to note that there is no universal script – we must tailor our approach to each patient and create a positive, trusting relationship. This is where motivational interviewing strategies come in.
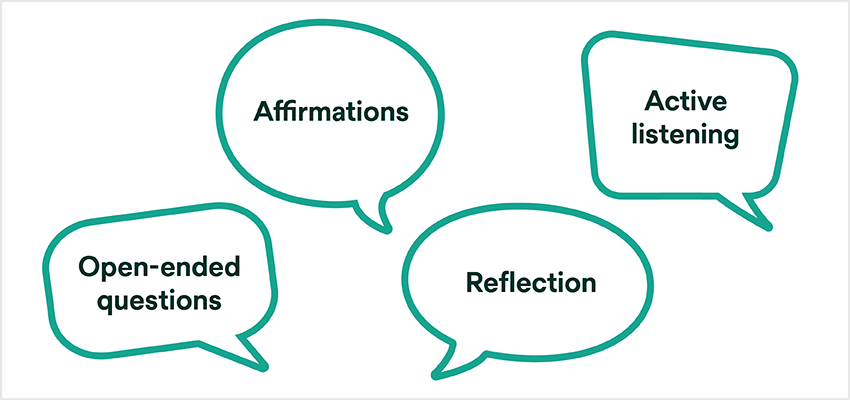
Motivational interviewing
Motivational interviewing (MI) has been a hot topic in dentistry in recent years, and for good reason. It’s a collaborative, goal-oriented style of communication centered on trust and empowering change – which fits right into a preventive mindset.
Traditional strategies involve approaching the situation solely from a biomedical perspective without considering the patient’s viewpoint, which can feel like lecturing. Motivational interviewing, on the other hand, emphasizes active listening and conversation. Using this communication strategy, clinicians should adopt an inquisitive mindset to better understand what motivates patients. Ask patients open-ended questions and engage them in a conversation rather than jumping straight to advice. Open-ended questions allow you to explore what the patient already knows without judgment. Listen carefully to their responses, look for non-verbal cues for more insight into their feelings, and take the time to reflect, clarify, or probe deeper if needed. Not only can you identify gaps in their knowledge, but you can often find clues to what’s standing in the way of positive change. For example, before I get into the technical part of the prophylaxis procedure, I always ask the patient how they care for their mouth, which products they’re using, and how it’s going. If you start with closed
questions like, “How many times do you floss?” patients may be tempted to lie and tell us what they think we want to hear. With a more curious, compassionate approach, patients are more likely to tell us what they are actually doing.
From there, acknowledge and reaffirm their efforts, strengths and successes before addressing issues or giving advice. By acknowledging what they’re doing right, you can help build their
confidence in their ability to change. For example, I might say, “You’re doing great and it’s clear your smile is important to you. Today I saw more plaque in your teeth, which is interesting
because I know you’re flossing. Can you show me how you floss, and maybe we can improve your technique?” It helps the patient see that you care. Patients will listen if they feel connected. Once you have this broader picture, you can coach, encourage, or guide your patients toward realistic goals that fit their unique circumstances.
This communication style gives patients an active role in their care, which ultimately helps build trust – and, eventually, better compliance. Using MI with a caries risk assessment can help patients see their progress in real-time – and may also lead to patients setting their own goals, making them much more likely to inact real changes. In fact, studies have shown that MI is “more effective in changing patients’ behaviors and improving their oral health compared to using traditional health education approaches that focus on disseminating information and giving normative advice.”2 Plus, a systematic review found that motivational interviewing strategies can help patients increase their oral health knowledge – which can improve oral health.2
Patients may refuse preventive treatments, such as fluoride, for various reasons, including a lack of understanding, oral health literacy, cost, time restrictions, or factors specific to the treatment, like flavor, mouthfeel, post-treatment esthetics, diet restrictions, or past negative experiences. Regardless, it’s essential to determine where the objection comes from. It’s very easy to go into “teaching mode” and lecture about what you know, but this may not address the issue at hand. Instead, use motivational interviewing strategies to listen, and let the patient know you care about what got them to that place. We can’t lead patients to a place of change without knowing where they are coming from. We also need to understand whether they’re receptive to change. Are they open to receiving new information? Would they be willing to try a new product that might be more pleasant? If not today, maybe next time.
From recommendation to results
As mentioned earlier, treatment will only be effective if the patient complies with our recommendations—which means we need to understand what will be most effective for the patient,
what motivates them, and what treatments or products are realistic for their unique circumstances. If your high-risk caries patient tells you time and again that they forget to brush, a nightly prescription toothpaste might not be the best treatment option at this time. Instead, you may want to consider a fluoride varnish at every appointment. Having personalized conversations to determine the best treatment plan for the individuals’ oral health conditions and what will work in their daily lives helps us motivate and inspire change.
We often recommend fluoride varnishes for children, but many of our adult patients can benefit from extra fluoride, too. Consider the type of fluoride you recommend based on each patient’s needs and conditions. For example, as patients age, issues arise with xerostomia and hyposalivation due to more medications and decreased salivary gland output. However, they need the minerals naturally available in saliva to achieve what we want with fluoride. In these cases, we must recommend a product that contains calcium and phosphate or one that delivers those minerals alongside fluoride.
If the patient doesn’t want to stick with our home care recommendations, we may have failed to make our suggestions personal, relevant, and important to them—but we can try again next time. We can’t change a patient’s habits in just one appointment, but the more open and understanding we are, the more open the patient may be to making changes down the road. For a deep dive into talking to patients about fluoride, check out our article: Fluoride and Your Patients – How to Start the Conversation.
Preparing your staff
While MI is a well-known strategy, it takes time and practice to learn and use effectively, which can be challenging in a fast-paced dental practice. To this end, many educational resources are available to help introduce and develop MI skills into routine practice. Studies have shown that MI training can help improve and build confidence in dental professionals’ patient communication abilities.2 Like introducing caries risk assessments, committing to personalized patient communication can help you develop strong relationships built on trust and improve acceptance and compliance.
The money question: Insurance
As dental professionals, insurance isn’t our favorite topic, but it’s an unavoidable part of working with patients—and often a significant hurdle to acceptance. However, we should never assume patients don’t want treatment because it isn’t covered. It’s always better to build a relationship with our patients, educate them, and present them with their options—including that while preventive care may not be covered today, it could save them substantial costs and natural tooth structures—so they can make an informed decision.
Patients sometimes ask: if you prevent cavities, won’t you be out of a job? But our job is to improve and maintain their oral health – we want healthy patients. Dentists and hygienists have a prevention mindset, and we must share that with patients so they understand that we’re on their side. Caries risk assessments and MI strategies help achieve our goal of creating healthy mouths by identifying high-risk individuals and tailoring preventive plans to their lives, including insurance coverage.
It all comes down to building a relationship of trust and working collaboratively with each patient. Every appointment is an opportunity to get to know your patients—listening, affirming, and checking their readiness to change—and fostering a solid connection. When used together, motivational interviewing and caries risk assessments can help you better understand your patients’ risk levels and their habits, lifestyle, and history on a deeper level. This strategy can help you hone your treatment recommendations, guide patients toward the best possible treatments individually, and empower them to make real changes for better overall and oral health.
SOURCES:
1. Gawel, Richard. “73% of Patients Have Lied to Their Dentist.” Dentistry Today, 30 Sept. 2021, www.dentistrytoday.com/73-of-patients-have-lied-to-their-dentist/.
2. Rogers KM, Arnett MC, Mays KA, Wang Qi, Blue CM. Dental hygienists’ use of motivational interviewing and perceptions of effectiveness in changing patient behaviors. J Dent Educ. 2022; 86: 909–917

How do you motivate your patients? Discover how caries risk assessments and motivational interviewing tactics can help you connect with…
Caries is a complicated multifactorial disease. In this two-part series, explore how caries risk assessments can help improve evaluation and…